The infectious liver disease hepatitis A has hit Appalachia hard during the past several months. But your risk of contracting the disease depends on several factors.
“So it’s very important to understand that there are certain groups of people that are at increased risk, as opposed to the general population,” West Virginia commissioner of public health Rahul Gupta said.
Up until this point, the outbreak in West Virginia has mostly affected people who are using illicit drugs (both injection and non-injection), people who are homeless or mobile, and those who have been recently incarcerated.
Basically, hepatitis A, a contagious liver infection, is transmitted by food, water, or personal contact with an infected person. But unlike its cousins hepatitis B and C, hepatitis A is not transmitted by needles and it does not cause long-term liver damage, nor does it become chronic. But it can make you very sick — mimicking major flu symptoms and making the afflicted jaundiced.
“We’re seeing that a little over 50 percent or a little over half of the population who exhibits symptoms are having to be hospitalized,” Gupta said.
And there’s no real treatment — you just, treat the symptoms. But there is a vaccine to prevent hepatitis A.
Although hepatitis A is not transmitted by needles, more than half of those infected have also tested positive for hepatitis B or C.
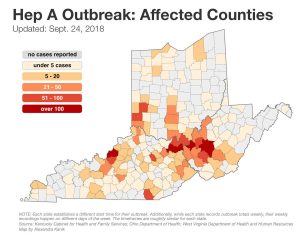
West Virginia is not the first state to report a hepatitis A outbreak. Michigan, California and Kentucky have also been hit, although neither Michigan nor California saw as many cases as Kentucky and West Virginia.
Kentucky’s outbreak started in August, 2017 — 1,788 cases have been reported to date. West Virginia’s outbreak began a few months later.
“We noticed our first case in January of this year. It has multiplied exponentially since then,” John Law, public information officer for the Kanawha-Charleston Health Department, said.
Since March 2018, West Virginia has seen 1,318 cases — about half of which are in Kanawha County. By comparison, in 2017, West Virginia reported six cases of acute hepatitis A.
Law said his department is trying to get a handle on the outbreak by partnering with organizations that are already working with illicit drug users and those experiencing homelessness, such as Covenant House and the free clinic Health Right.
“As a collaborative effort, then, we sent out a letter with the health department to all the shelters, etc., encouraging them to have every new client come through Health Right to have like a established physical just to check them over and screen them for any kind of vaccinations and hopefully give them hepatitis A vaccination then,” Angie Settle, Health Right’s executive director, said.
She said they also went to some of the local recovery centers and did mass hepatitis A vaccinations. So far, Settle said Health Right has given close to 2,000 vaccinations. The DHHR has distributed more than 24,000 vaccines statewide.
So do you need a vaccine? If you work in food prep, or come in close contact with those at risk, it’s probably wise. And if you don’t, one of the best ways to protect yourself is just to wash your hands frequently, especially after using the bathroom.
This article was originally published by West Virginia Public Broadcasting.



