As rates of coronavirus (COVID-19) infection and death continue to rise, it is important to consider how rural areas may be differentially affected.

On the one hand, rural parts of the U.S. may be comparatively better off than urban places due to lower population density in rural areas. Lower population density reduces opportunities for virus spread.
On the other hand, there are several features of rural populations and places that increase their risk of coronavirus-related mortality and other long-term health impacts.
These include the realities that rural populations are older and have higher rates of several chronic health conditions, and rural areas have a less robust health care infrastructure to deal with coronavirus cases.
Rural economies may also be affected in different ways than their urban counterparts, which has implications for long-term rural population health outcomes.

Rural Populations Are Older
Coronavirus infection is more deadly for older adults. According to a recent CDC report, thus far, 31 percent of COVID-19 cases, 45 percent of hospitalizations, 53 percent of intensive care admissions and 80 percent of deaths have been among adults aged 65 and older, with the highest percentage of severe outcomes among those 85 years and older. This is bad news for rural America. Nineteen percent of the rural population is 65 years or older, compared with 15 percent in urban areas. Whereas the average share of the population that is age 65+ is only 15.2 percent among large metropolitan counties, the average share of the population that is age 65+ is 21.7 percent in the smallest nonmetropolitan counties (see Figure 1). Nearly two-thirds of the U.S.’s 643 small metropolitan counties are considered “older-age counties”— counties where more than 20 percent of the population is age 65 or older (see Figure 2). Only 7 percent of large metropolitan counties fall into this category.
In addition to its implications for mortality rates, the older age structure in rural areas has implications for informal caregiving. Older adults nationwide rely on informal caregivers (e.g., friends, family, neighbors) for support, but access to informal caregivers may be more difficult in rural areas given longer travel times. This may lead to greater isolation among older adults in rural areas and may mean that they do not get necessary healthcare services and other essential resources, like medications, groceries and social interaction.
Higher Prevalence of Chronic Health Conditions
Early data from China [PDF] show that people with certain serious chronic medical conditions, such as heart disease, diabetes, chronic respiratory disease, lung cancer and depression are at greater risk of death and other serious complications from COVID-19 because these conditions weaken the body’s health defense and immune system against viral infection. Rural Americans have higher rates of each of these chronic health conditions than their urban peers (see Figure 3). This means that although transmission rates may be lower in rural areas, the percentage of cases resulting in death and other serious complications could be higher in rural than in urban areas.

More Limited Health Care Infrastructure
Since 2010, 126 rural hospitals across 31 states have closed. Even when hospitals are available in rural areas, they do not have the capacity to deal with a surge in coronavirus cases, and they have limited availability of medical personnel, ventilators, personal protective equipment (e.g., masks, gloves, gowns), and other essential supplies. Particularly concerning is that only 1% of the nation’s ICU beds are located in rural areas. In addition, rural physicians are older than their urban counterparts, meaning that they are at very high risk while providing services.
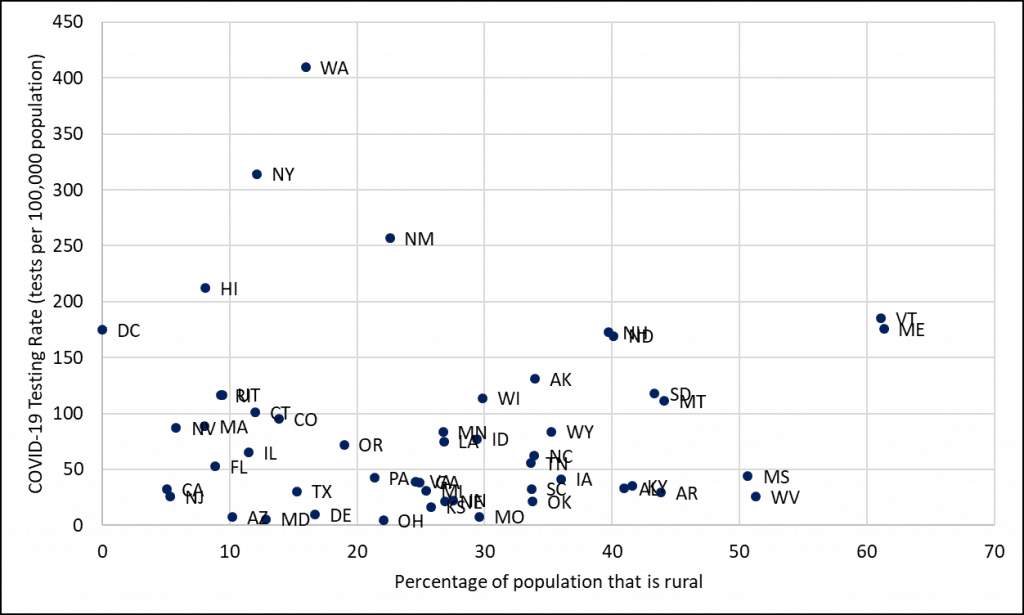
Besides the resources that are necessary to treat the virus, COVID-19 testing availability and access is also essential because a) federal and state governments need to know where to allocate limited treatment resources and b) individuals may be more likely to self-isolate if they know there are positive cases in their communities. Moreover, people who do not know they have the virus because they have not been able to get tested may inadvertently pass the virus on to someone else. This was especially likely in the early stages of the pandemic before social distancing protocols had been widely adopted. By all accounts, the availability of tests for COVID-19 has been abysmal nationwide, but especially so in rural areas. In general, testing rates have been lower in the most rural states (see Figure 4). The exceptions are Maine, New Hampshire, North Dakota, South Dakota and Montana – all of which are at least 40 percent rural and currently have above average testing rates. High-volume mobile test collection sites are popping up in high population density areas on a daily basis, but most rural residents live hours from these sites. Some rural hospitals have converted office space normally used for other medical purposes into COVID-19 testing spaces, but this has varied significantly across the U.S.
Longer-Term Health Consequences
There are also potential longer-term consequences to rural population health. The connection between local economic conditions and population health is well-documented. The Great Recession, which represented a severe and sudden economic downturn, was associated with higher population-level rates of poor self-reported health, disability, problems with digestion and sleep, diabetes, low-weight births, psychological distress, suicide, higher caloric intake and declines in physical activity and fertility. A 2016 review by Claire Margerison-Zilko and others also shows that alcohol consumption, problematic drinking and smoking increased among individuals who lost their jobs during the Great Recession.
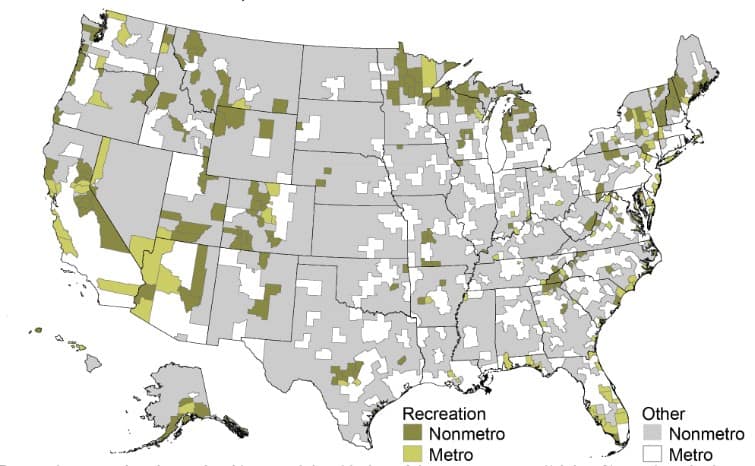
Not only have rural economies not yet fully recovered from the Great Recession, but rural economies tend to be less diversified than urban economies, increasing risk of widespread job loss if that industry goes under. Nationwide, there have been massive layoffs in restaurants and bars, hotels, entertainment venues and other hospitality venues. Places where a large share of employment and wages are coming from these types of businesses will be very hard hit. Rural counties are more likely to be dependent on these recreation-based industries (see Figure 5). Eighteen percent of small nonmetropolitan counties are economically dependent on recreation compared to only 10 percent of large metropolitan counties (see Figure 6). This means that rural economies may be harder hit by business closures and unemployment and the subsequent negative health outcomes of these economic downturns.
Many rural hospitals, already stretched thin and on the brink of closure, may not survive from the financial hit of the coronavirus. Cancellations of regular doctor’s visits by fearful patients and postponement of “non-urgent” elective medical procedures to prepare for a surge in coronavirus cases means that these hospitals are missing out on a substantial portion of their regular revenue. At the same time, hospitals are finding themselves in a position to expend precious funds on high-cost personal protective equipment, such as masks and other essential resources. Many rural hospitals will not be able to withstand these financial losses for very long before shutting down for good.

Conclusion
In sum, several features of rural populations and places increase the chances that we will see high rates of COVID-19 mortality and other long-term health consequences in rural areas. However, not all rural places and populations are the same. Demographic and economic characteristics, health care capacity, economic resources and policy responses vary widely across different rural communities. Responding quickly and comprehensively, even before a particular geographic area has any confirmed cases, will save lives.
Finally, the impacts of the coronavirus epidemic on rural communities will also have major implications for urban populations. Rural America supplies disproportionate shares of the nation’s food, energy, military personnel and natural amenity recreation. These are resources that urban America depends upon. Rural, urban or somewhere in between – we are all in this together.
Shannon Monnat is the Lerner Chair for Public Health Promotion, associate professor of sociology, and co-director of the Policy, Place, and Population Health Lab in the Maxwell School of Citizenship and Public Affairs at Syracuse University. This research brief was originally published by the Lerner Chair for Public Health Promotion.
This article was published by The Daily Yonder.



