For years, Wendy Gooditis tried to help her older brother Brian access medical care. When he was just 11 years old, he suffered a horrific trauma at the hands of someone outside their family, which resulted in post traumatic stress disorder, or PTSD. Brian’s condition was undiagnosed for much of his life — until about five years ago.
One of the hallmark symptoms of PTSD is terror, particularly at night, something Gooditis said plagued her brother. Early on, Brian found that alcohol brought some relief to his terror-filled, sleepless nights. As an adult, the combination of PTSD, alcoholism and lack of proper care for either condition made his life difficult. In attempting to find adequate healthcare for her brother, Gooditis learned how challenging accessing care in the state of Virginia could be.
“When Trump was inaugurated in 2016, I thought, ‘This administration is not going to do anything to help people like my brother,’” Gooditis said, “and I decided then that I had to do something to fix this situation.”
She announced her candidacy at the end of February 2016 for a seat in the Virginia General Assembly. Two weeks later, she found her brother dead. He was 57 years old and Gooditis is haunted by the question of what his life might have been like if he’d had appropriate medical care.
“I had $500 and…just me, as far as my candidacy,” she said. “It would have been so easy to quit. But, at this point, I’d met so many people like my brother. I made it my mission to help.”

Gooditis was elected to the House in 2017 and when she got there, she wasn’t the only person who wanted to change healthcare in the state.
In late May of 2018, Virginia’s General Assembly passed a budget that included Medicaid expansion, a provision of the federal Affordable Care Act, or ACA, that allowed states to choose whether to allow people at a slightly higher income to be eligible for the program. Governor Ralph Northam signed the bill on June 7 last year and on January 1, 2019, some 400,000 residents of the state will be eligible to enroll in Medicaid.
Healthcare facilities across Virginia are beginning to prepare for the new population that is eligible for coverage under the federal program. At the same, though, the current presidential administration is working to dismantle the ACA, the law that made expansion possible. In many ways, the situation in Virginia reflects the national turmoil over the access and affordability of healthcare.
For Virginia’s Free Clinics, Medicaid Expansion Is a Double-Edged Sword
On its face, Medicaid expansion seems like good news for clinics whose mission is to provide care for those who may not otherwise be able to afford it. Although qualifications vary from state to state, in Virginia the expansion population will include people who make up to 138 percent of the federal poverty level. For a family of four, that’s $42,435 per year in 2018.
Many of those Virginians are using the services currently available at free clinics. That means, upon their enrollment, Medicaid could be a new source of income for these healthcare providers that typically rely on grants and donations to serve their client population. But these clinics will face significant challenges as they prepare to serve patients who are newly covered by Medicaid.
The Virginia Association of Free and Charitable Clinics, VAFCC, provides a range of services for free clinics, such as technical assistance, training, advocacy and resource development. There are about 70 free and charitable clinics in Virginia; 63 are members of the VAFCC. Only about 10 of those members will accept Medicaid initially. The rest are evaluating their infrastructure, patient population and community needs before reaching a decision.
CEO of VAFCC Linda Wilkinson said whether a health clinic will begin accepting Medicaid depends on multiple factors. One is whether they have the appropriate infrastructure internally to bill the federal program for the services they provide newly enrolled Medicaid patients. Another is whether these patients will have an alternative provider in their community to turn to should the clinics choose not to accept Medicaid.
For some clinics, creating a billing infrastructure will take significant investments in the hardware to complete the process, like computer software and electronic records systems, but also could mean adding additional staff trained in the process, which can be expensive.
When it comes to access, roughly half the state is classified as being medically underserved by the Virginia Healthcare Association. That means there are too few primary care providers, a high infant mortality rate, or a large population of elderly people, according to the Health Resources and Services Administration. In addition, many areas of Virginia are considered health professional shortage areas, where there aren’t enough providers to serve the population.
Whether there are enough providers in any given community can be a politically-charged issue, but so can the eligibility requirements. Wilkinson said about 100,000 Virginians who earn between 139 percent and 200 percent of the federal poverty level will remain uninsured. Some clinics will continue to provide free or charitable care and serve that segment of the population.
The Sinclair Health Clinic says its Decision is Made
The Sinclair Health Clinic in Winchester, Virginia, is one of the 10 VAFCC member clinics that intends to begin accepting Medicaid in January. Since approximately 80 percent of the clinic’s patients will be eligible for the program under expansion, the decision was a foregone conclusion for Executive Director Brandon Jennings for a couple of reasons. For one thing, there aren’t enough providers in the area to absorb that many new patients.

“We would basically kick 1,600 patients out of our clinic because they’d no longer meet our eligibility criteria,” Jennings said of the patients who would be Medicaid eligible, “and there’s no one in town to pick them up.”
“Having 1,600 patients on day one needing to find a provider would be downright impossible for a town of our size, and I would argue [that would be true] for a lot of towns in Virginia,” Jennings said. The clinic was already having trouble placing clients with specialists before Medicaid expansion became an option, he added.
Even though the clinic will accept Medicaid, Jennings said patients will ultimately have more control over what doctor they can see. Without expansion, most of them can’t afford to see another provider.
“There’s no reason they have to stay with us,” Jennings said. “They can move down the street if they can get in to see another provider, and some may very well do that.”

But, the decision to begin accepting Medicaid means the clinic will need to make some fairly drastic changes to how it operates. Care is currently provided free of cost to all patients so there is no billing department at the Sinclair Health Clinic. As a facility that accepts Medicaid, however, they will need to bill Medicaid, but that’s not necessarily a simple task. Healthcare is a heavily regulated industry and the Centers for Medicare and Medicaid Services has strict regulations that all practices who bill them for services must abide by.
“There are usually, depending on the practice size, anywhere from one to five people sitting in the back,” Jennings explained of a typical physician’s office, “and the only thing they’re doing is billing and discussing with insurance companies about ways to get claims paid. We don’t have any of that built in.”
But the Sinclair Health Clinic has at least one advantage as they shift to accepting Medicaid: two of their staff members previously worked in practices that billed, although not specifically Medicaid. Still, there will be challenges in building an infrastructure to handle billing. The clinic has been working with Athena, the company that supplies their electronic medical records system, which has a billing component.
Medicaid will Work for Sinclair, But Not for Everyone
The challenges the Sinclair Health Clinic is facing in the wake of Medicaid expansion is similar to that of other free clinics across Virginia, including the Health Wagon in the Appalachian Mountains of southwest Virginia.
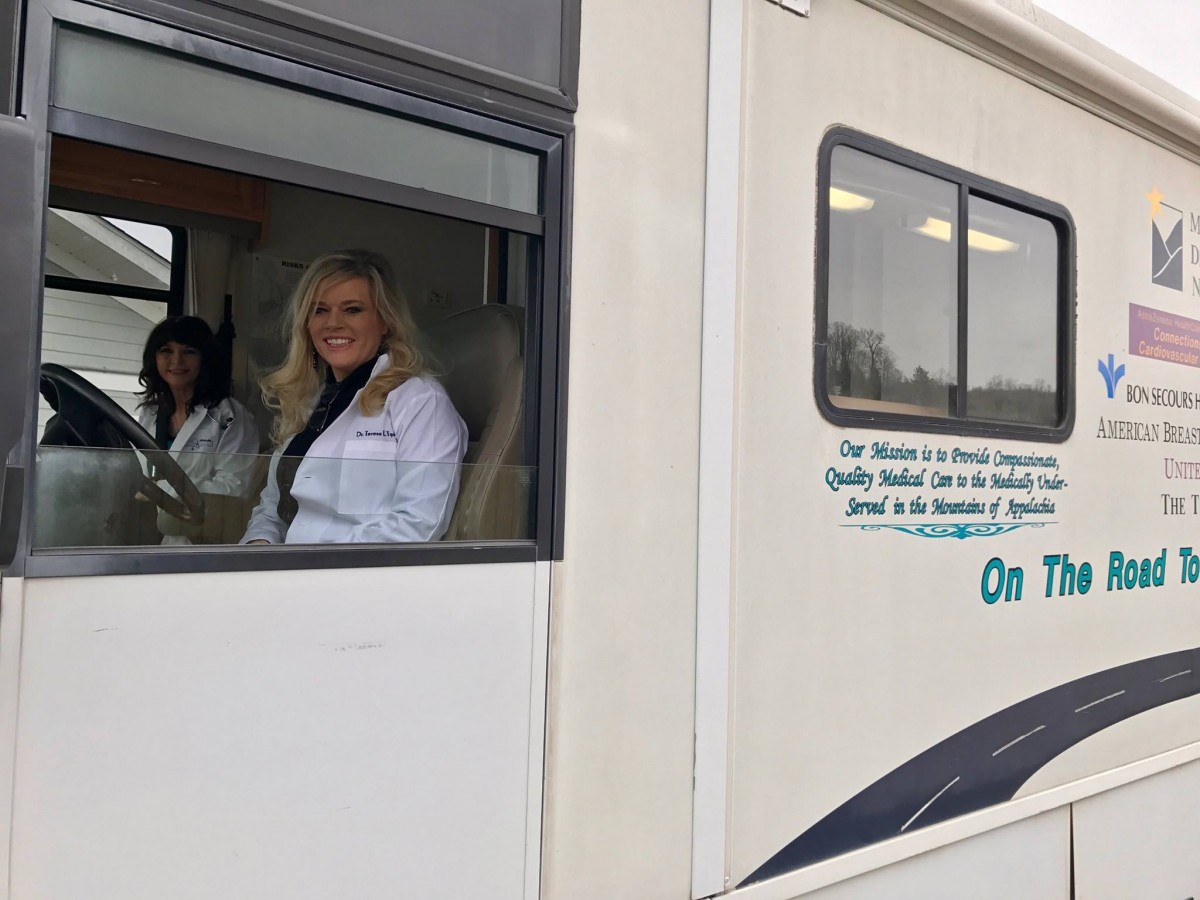
Clients of the Health Wagon usually don’t have health insurance, often live in chronic poverty and many have low educational attainment. Preliminary estimates at the Health Wagon show that about 50 percent of their clients served by their one mobile and two brick-and-mortar clinics will become eligible for Medicaid under expansion. Executive Director Dr. Teresa Gardner Tyson stresses that those are very early estimates and said she expects that number to grow.
The organization partners with Remote Area Medical (RAM) each year for the Remote Area Medical – Wise Health Expedition, the largest medical outreach of its kind in the country. The program provides free health, vision and dental care at what’s usually a one day event. People arrive sometimes days in advance to wait in line to get care they otherwise would be unable to access.
Tyson contends that the free event, held every July, was instrumental in the political shift in the state that led to Medicaid expansion.
“We’ve spearheaded that [event] for the last 19 years,” she said. “For the last five years, the Health Wagon has invited all legislators, Democrat and Republican both, to come and look at what we face here in Appalachia. We’ve invited these politicians to come and see people lining up when we open the gate. We give out about 1,700 numbers on that Friday by 5 a.m.”
People who come after that, Tyson said, are turned away.
“I think it’s been very eye-opening for them,” Tyson said. She wants politicians to understand that in the United States, in 2018, people sometimes arrive a week in advance to get healthcare.
“This is happening in central Appalachia, where we need more focus to help us turn around healthcare disparities here in the mountains,” she said.
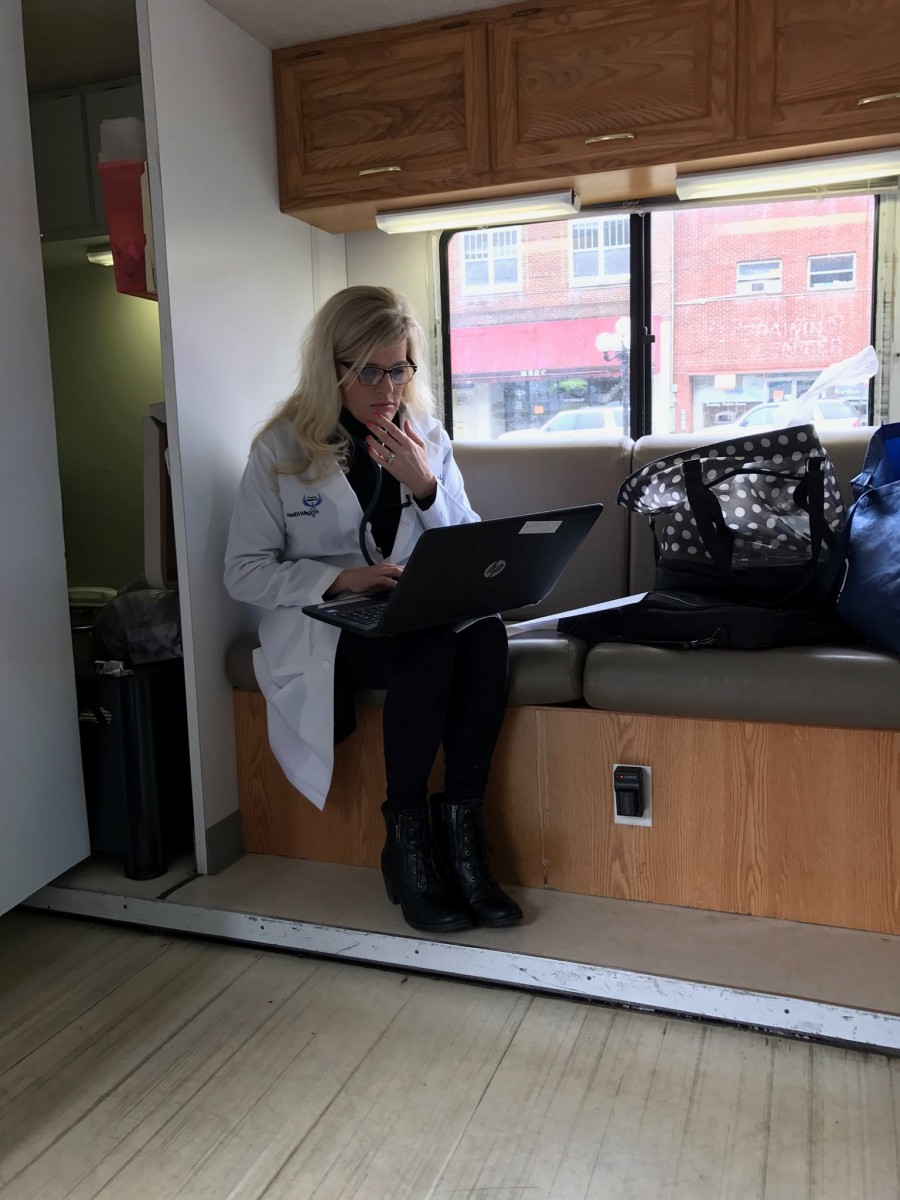
Although Tyson said her organization is in the preliminary stages of determining if they will accept Medicaid, the Health Wagon faces the same challenges as the Sinclair Health Clinic. Medicaid billing would also be a new practice for the nonprofit, but Tyson said the Health Wagon is considering an alternative approach. Rather than changing the way the two existing clinics operate, the Health Wagon may add a third physical location to solely serve the newly expanded Medicaid population.
“It’s a very real possibility that we’ll open up a rural health clinic and get those patients into care there,” said Tyson.
There is perhaps an additional obstacle for the Health Wagon, though– the culture of their clients.
In addition to billing CMS for services, practices that accept Medicaid must also send a copy of that bill to the patient. Patients aren’t required to pay anything, but Tyson is worried that some of the population she serves might not understand that. After all, they currently receive their healthcare free of cost and never have to look at a paper bill.
“From a cultural perspective, if they receive that [Medicaid statement], it might be a barrier for them to returning for care if they thought they owed a bill and they weren’t able to pay it,” she said.
Enrollment Challenges
Before either the Sinclair Health Clinic or the Health Wagon can begin seeing Medicaid patients or billing for services, eligible patients have to apply to actually receive Medicaid benefits. And the application is complex.
Jennings, with the Sinclair Health Clinic, said their staff has been completing mock applications so they can understand what their clients will be facing, and so far, even the healthcare professionals on his staff have been confused. That can potentially mean problems for this population, Jennings said, some of whom struggle with literacy.
“We’re not being resourced to help with that at all, and so it’s a problem,” Jennings said. “Yet, we need to [help people apply] as part of the community because our patients need to enroll for the full benefit.”
Just being eligible for coverage under Medicaid expansion isn’t enough, Jennings said. Patients must be enrolled in the program to receive coverage.
The Health Wagon has applied for a grant to fund two eligibility coordinators to help clients apply for Medicaid.
“We want to get our patients into the system so that they have access to the care we have long championed for,” Tyson said.
The VAFCC has some resources available to help clinics handle this aspect of expansion, according to Wilkinson. She also said the Department of Medical Assistance Services, the Virginia State Department of Social Services and coverVA.org are doing excellent, and necessary, work to make residents aware of their potential eligibility, as well as help them apply.
“Some patients may have health insurance for the first time in their life,” she said, but issues with the application and technology may pose a problem, just as they did in the early days of the ACA.
When the online marketplace to purchase insurance through the ACA was initially rolled out under the Obama administration, results were disastrous. Headlines in early October 2013 included: “Tech Problems Plague First Day of Health Exchange Rollout” from NPR and “How Long To Fix Obamacare Tech Problems? Long” from CNBC, among many others.
Technical glitches in the Healthcare Exchange have continued over the years, but now, the Trump administration is committing fewer resources to helping enrollees work through those problems. Even so, approximately 11.8 million people signed up for coverage under the ACA in 2018 and around 27 percent of them were new to the program.
The Bigger Picture
The fact that Virginia, once a reliably red state, is now decidedly purple may be due in large part to the issue of healthcare. It spurred Gooditis to run for office, and several Republican lawmakers joined Democrats in the vote earlier this year to expand Medicaid in the state.
“I came to the conclusion, for me and my district, that ‘no’ just wasn’t the answer any longer,” Republican State Senator Ben Chafin told the New York Times in May. Chafin represents the area served by the Health Wagon in southwestern Virginia.
“Doing nothing about the medical conditions, the state of health care in my district, just wasn’t the answer,” Chafin added.
Chafin is not alone in his stance. Other Republicans are also changing how they talk about healthcare.
The Washington Post reports that in 2014, 84 percent of ads about healthcare from Republicans or from organizations affiliated with the Republican party, attacked the ACA. In current midterm campaigns, Republicans seem to be avoiding the issue of healthcare altogether.
“Yeah, we probably can’t talk credibly about repeal and replace anymore,” Republican Congressman Tom MacArthur of New Jersey told the Post.
Notably, there’s nothing about the issue of healthcare on Virginia Congresswoman Barbara Comstock’s website. Comstock represents the 10th district, which includes Winchester, where the Sinclair Health Clinic is located. In 2014, her campaign platform included repealing and replacing Obamacare. Comstock’s office did not respond to a request for an interview for this article.
In four states, Montana, Nebraska, Idaho and Utah, Medicaid expansion will be on the ballot in November. The Fairness Project, a grassroots organization that supports economic fairness, is working with groups in those states to give voters a voice in the debate.
“Ballot initiatives are powerful because they strip away the political theater and partisanship, cut out the lawyers and lobbyists and give voters a clear, direct way to help their families and their neighbors,” said Jonathan Schleifer, executive director of the Fairness Project, via email.
Despite the problems that Medicaid expansion will create for free and charitable clinics in the state of Virginia, many administrators and advocates are enthusiastic about more people being able to access healthcare, including Sinclair Health Clinic’s Jennings and the Health Wagon’s Tyson.
The two will continue to consider how changes to their billing and operational systems will impact their patients and clinics over the next few months, and will handle events outside of their control as they happen.
“This is the boat we’re in,”Jennings said. “We’ve got to figure out how to make it float.”



