The opioid crisis gripping the Ohio Valley is now, according to President Donald Trump, a national emergency. But more than a week after the president made that announcement, state and local health officials in the region told the Ohio Valley ReSource that they have little information about what that emergency declaration actually means, or what additional tools it might provide.
A White House spokesperson indicated the substance of the emergency declaration would go beyond the recommendations of a presidential commission’s recent report but that the plan was still under review.
Meanwhile, addiction treatment specialists and public health officials have no shortage of ideas for what they would like to see from the federal government to help them combat the worst drug crisis most of them have ever encountered.

Emerging Emergency
Kentucky’s Office for Drug Control Policy Director Van Ingram said he had no information on when the emergency declaration might have effect on the ground. He said he did not have direct contact with members of the president’s commission on the opioid crisis, but has long been discussing the opioid epidemic with both Kentucky Gov. Matt Bevin and elected officials at a federal level.
Ingram said many elements in the 10-page draft document released by the commission are already in place in Kentucky.
“None of this is new to us,” he said. But he said the national focus and attention will help.
“This is an all hands on deck problem and the leadership has to come from the top,” he said.
The federal government has declared other national health emergencies in recent years, but officials warn that the opioid crisis presents unique challenges.

A 2009 emergency declaration was called because of the H1N1 flu. There’s now an ongoing emergency concerning the Zika virus. The emergency system federal health officials follow is effective for these types of medical crises, which require mobilizing stockpiled vaccines and other supplies to communities as quickly as possible.
But the system is not designed for the more complex problems created by an opioid epidemic.

West Virginia State Health Officer Dr. Rahul Gupta has been practicing for 25 years. He calls the opioid crisis the worst health crisis he’s dealt with because it affects nearly every aspect of the social fabric: individuals struggle with addiction, grandparents have to raise children displaced by addiction, and courts are slammed with drug-related cases.
For this reason, he said, any plan of action resulting from an emergency declaration needs to be broad, but with clearly defined, achievable goals on a timetable.
“So that we as a nation are moving towards common goals with the hope of reducing both the overdose deaths as well as the level of addiction,” Gupta said.
Immediate Needs
Treatment specialists hope for more federal money for medications used to combat addiction.
Agencies have treatment medications on hand but the costs of those medications are increasing with the rising overdose and addiction rates.
Kim Miller, Director of Corporate Development with Prestera Center in Huntington, West Virginia, said the monthly injection medication Vivitrol is a good example.
“When it came on the market, it was about $400 a month. Now it’s up to $600 a month,” she said.

CREDIT REBECCA KIGER
The federal government could tap into emergency funds, depending on what route President Trump takes with the emergency plan. But some of those reserve funds are limited.
For example, the Public Health Emergency Fund has had varied amounts appropriated by Congress. It once held $45 million, according to a 2008 report. At one point last summer, during the Zika emergency, it only held $57,000.
The president’s commission on the opioid crisis wrote last month that a national emergency declaration could pressure Congress to provide more funding in the federal budget.
Medicaid Role
Health policy experts agree with another of the commission’s recommendations to expand how Medicaid pays for substance abuse treatment.
Alex Shekhdar is the vice president of federal and state policy at Medicaid Health Plans of America, the trade association representing the managed Medicaid industry.
He said overturning what is known as the exclusion on IMD, or Institutions of Mental Disease, could help increase the number of treatment beds available in areas hardest hit by the crisis.
The exclusion was was put into place in the 1960s. At the time, Shekhdar explained, mental health treatment was moving toward services more integrated in the community and away from large institutions, which were often little more than warehouses for the mentally ill. The rule limits mental health facilities that can receive Medicaid reimbursements to 16 beds.
But that well-meaning rule is now limiting the ability to expand some substance abuse treatment facilities.

Since 2015 states with the highest overdose rates, including many in Appalachia, have petitioned the federal government to waive the exclusion. Kentucky has a waiver application pending.
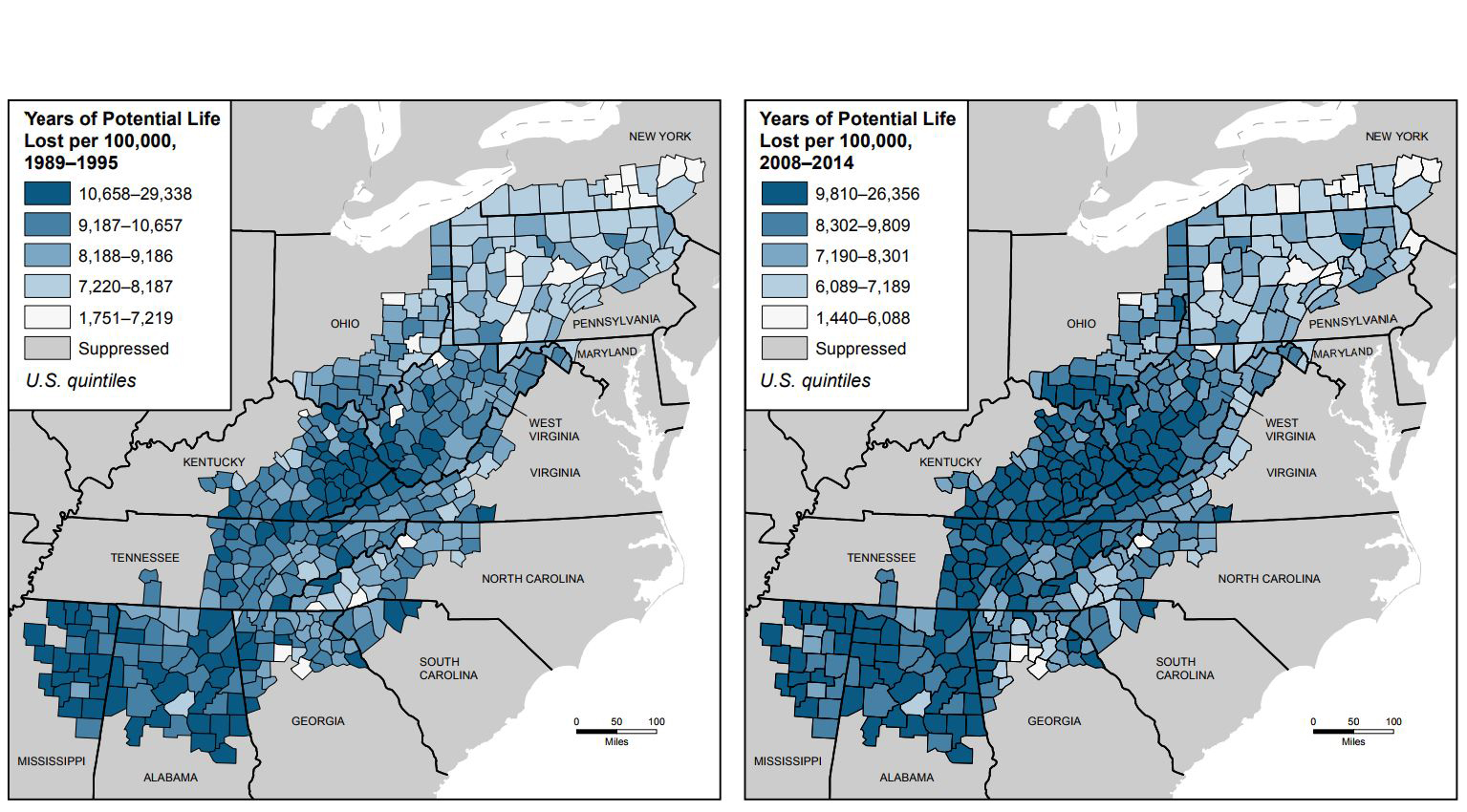
Explore our interactive county-by-county overdose map for Kentucky >>
Kentucky’s Van Ingram said his state’s waiver could be approved this fall. Ingram said it’s critical to get more beds so that when a person suffering with an opioid problem can get treatment when they reach “that moment of clarity where they want to get help.”
More Than Money
Increasing treatment beds also brings the need for more qualified addiction specialists, something the president’s commission did not address in its initial report.
The Prestera Center’s Miller said her organization has been able to secure the resources to run the Prestera Center’s comprehensive, evidence-based addiction treatment. But they have recruiting issues tied to the crisis.
“Doctors are just not excited about working with those folks because they can be difficult to work with,” she said. “And the same is true for counselors, we have a counselor shortage.
Click here to read more of our coverage on the opioid crisis >>
There is precedent for sending public health workers to crisis areas in times of a health emergency. But it’s unclear if those workers would be trained to deal with addiction treatment.
No More “Just Say No”
When the President spoke about this issue he emphasized the role for law enforcement. Trump’s comments struck many as similar to the “Just Say No” campaign of the 1980s.
“If they don’t start, they won’t have a problem,” he said. “If they do start, it’s awfully tough to get off. So if we can keep them from going on and maybe by talking to youth and telling them, ‘No good, really bad for you in every way.’”
Recovery specialists are concerned this signals that a similar program will be rolled out as part of the emergency declaration.
Matt Boggs with Recovery Point in Huntington said that the “Just Say No” approach was well intended but just not effective because it didn’t take into account that addiction is a disease.
“If someone wasn’t able to say no, they felt like a moral failure,” he said. “We’ve got to continue to teach kids why they say no and how to deal with all of the issues they’re going to face.”

Boggs and others working with those with substance use disorders say they want evidence-based education and prevention programs that focus on public health rather than law enforcement.
Kentucky’s Van Ingram, a former police chief, said the traditional “law and order” approach isn’t the answer. The current epidemic is two decades in the making. Law enforcement efforts alone are failing to stop the spread of the disease and ever-rising number of overdose deaths.
And although Ingram knows many people feel overwhelmed at the complexity of the problem and scope of the devastation, he emphasizes that there is hope.
“People do recover. I meet them every day,” he said. “People do turn their lives around and do amazing things with their lives.”