This is the third story in Critical Condition, a three part series. Read more here.
“I’m hopin’,” Andrea Haas says with conviction.
The Remote Area Medical clinic has come to Jellico, Tennessee, in Campbell County, on the Kentucky border. It’s offering free health care.
Haas’s hope for today is that her teeth will get pulled. She’s suffered all her life from grand mal seizures, and with each episode she bites her tongue. “They said one wrong, good bite and I could lose my tongue,” Haas says. The plan is to extract her teeth and, later, replace them with better-fitting dentures.
It’s 9:30 a.m. Haas, 31, arrived last night. The gates opened at midnight, the clinic doors at 6 a.m. It’s first come, first served.
All manner of health care services are in limited supply in this part of central Appalachia. In March, Jellico Medical Center, a 54-bed acute-care hospital, officially shut down after not having admitted a patient since November.

It’s an increasingly, depressingly common story. Communities across Appalachia, as across the whole of rural America, are struggling to maintain hospital care. Rural hospitals are closing at an alarming rate – 138 since 2010, according to research from the University of North Carolina, with a record high of 19 in 2020.
There are a number of reasons why: Rural hospitals operate under perilously tight margins; many are in the red. Buildings and equipment are commonly old and costly to maintain. Rural hospitals serve declining populations – young people leave in search of opportunities – populations that are, on average, less healthy and of lower income, with a higher percentage who are under- or uninsured.
Campbell County ranks 93rd worst in health outcomes of Tennessee’s 95 counties and has a poverty rate approximately double that of the nation.
“I’m hopin’,” Haas repeats, this time in reference to the hospital reopening. She worries about those who now must drive almost an hour to Knoxville or across the border to Kentucky to see a doctor, and even more about those with no means to make the trip.

There is some encouraging news. An Indiana-based health care system, Boa Vida Healthcare, has reached an agreement with Jellico’s city council to reopen the hospital, reportedly within the next six months. Still, local residents have been conditioned not to get overly optimistic. The previous owner was around for just two years.
COVID-19 took an incalculable toll on rural communities. In the first months of the pandemic, says Jacy Warrell, executive director of the Rural Health Association of Tennessee, “a lot of rural communities thought it was a bigger-city issue and that they didn’t have to worry about it because they were more isolated.”
But when it did hit, it spread quickly. By September, the death rate in rural America had surpassed that of urban centers.
Tennessee’s hospitals, like those across the nation, experienced a dramatic drop in revenue throughout the pandemic and continue to lose money. A recent American Hospital Association report estimates the pandemic could cause hospitals to lose as much as $122 billion this year.

Tennessee has experienced more rural hospital closures per capita than any state. In 2018, the state legislature passed the Tennessee Rural Hospital Transformation Act to support rural hospitals “in assessing viability and identifying new delivery models, strategic partnerships, and operational changes” to support health care services in rural communities.
Consultants were sent out to meet with rural hospital administrators and other community leaders. Essentially, what they told them, says Randall Rice, board president of the Tennessee Health Care Campaign, was that they needed more money. “That was not a revelation,” he says.
More money is certainly required. So, too, is a more strategic, integrated approach to rural health care. Andrea Haas knows she and her neighbors deserve better.
Reverberating Consequences
The recently departed owner of Jellico Medical Center was Florida-based Rennova Health. Rennova also previously operated Jamestown Regional Medical Center, an hour and a half to the west along Tennessee’s Cumberland Plateau, but shuttered it in June 2019.
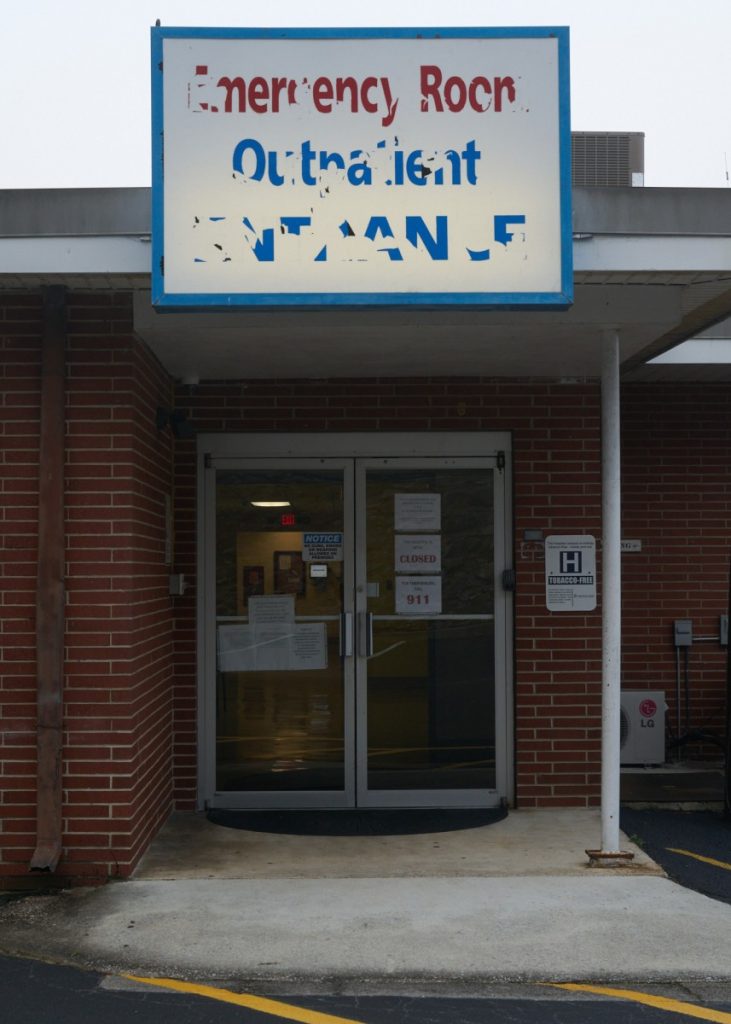
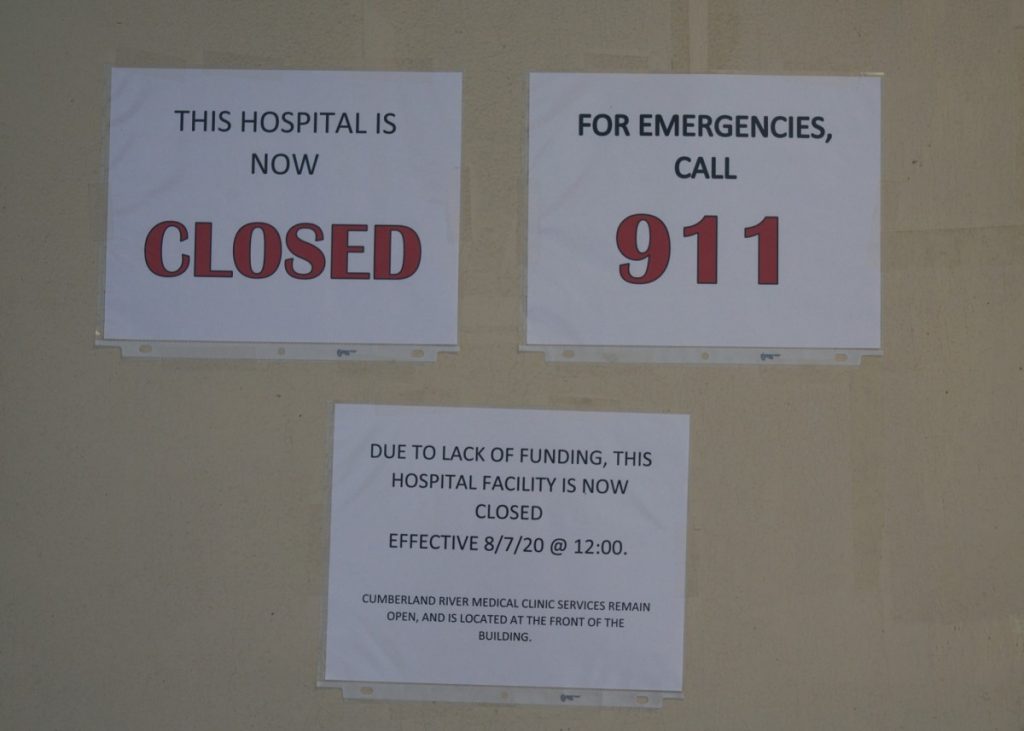
A third hospital, Cumberland River, in the Clay County town of Celina, 45 miles northwest of Jamestown, closed in March 2019, temporarily reopened, then closed again last August. (It was not owned by Rennova.)

Rennova Health still operates Big South Fork Medical Center in the Scott County town of Oneida, about halfway between Jellico and Jamestown. The hospital has closed twice in the past decade and is now a shell of what it once was. There’s no longer intensive care, surgery, obstetrics, or geropsychiatric care. For a time, there were no inpatient beds; six have only recently been made available.
Today, the hospital’s only doctor, Deepak Reddy, lives in the facility to be immediately available around the clock.
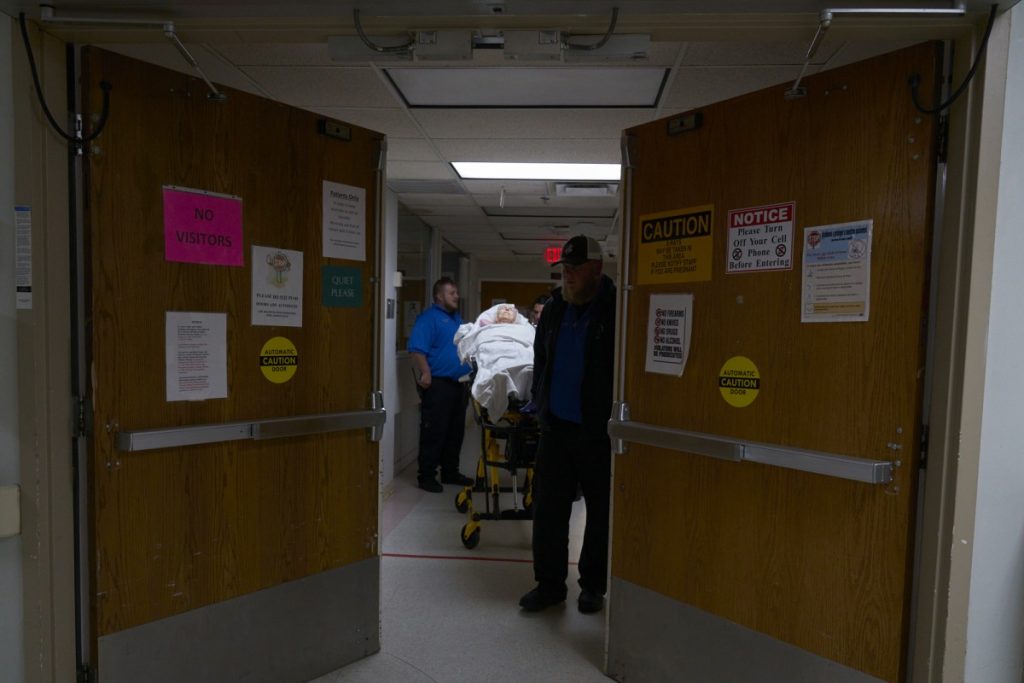
Big South Fork Medical Center employees recently reported – not for the first time – that the company was behind in issuing paychecks, and that a number of them wouldn’t be returning to work until paid. This follows a pattern from Jellico Medical Center, where in February employees reported being unpaid and quit their jobs, creating a staffing crisis. Ambulances were diverted from the emergency room to neighboring hospitals, 45 minutes to an hour away.
The consequences of a closed or minimally operational hospital reverberate throughout the community. Some of those consequences are immediate.
Scott County generally has two ambulances in service at a given time. Paramedic Alison Jeffers says that if either has to transfer a patient out of the county, “You’re looking at two and a half hours minimum – and that’s if everything cooperates, there’s beds at the facility, traffic’s good – two and a half hours minimum before we get back into town.”
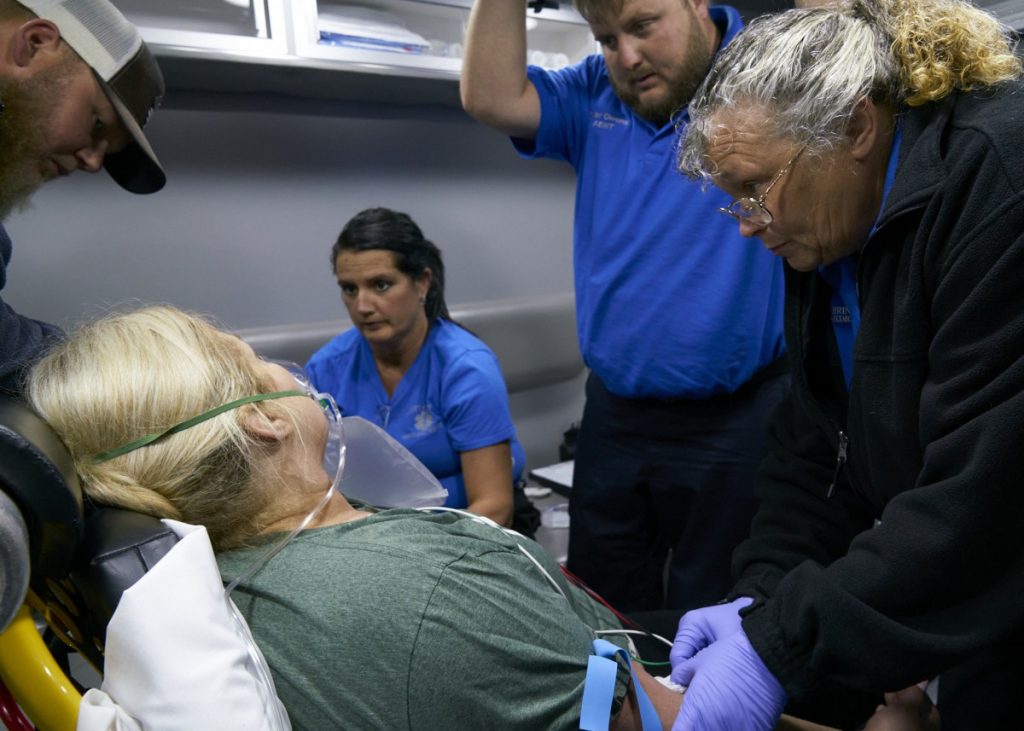
Moreover, that travel time can be the difference between life and death. For patients in trauma, the first hour is known as the “Golden Hour,” after which the risk of death increases dramatically.
Other consequences have longer-term effects. Pam Thompson is a behavioral-health counselor with Mountain Peoples Health Councils, a nonprofit community health center in Scott County. When she moved back to the county, she considered starting a private practice, but the hospital had shut down. Without emergency services for clients in crisis, she elected not to open her own practice.
Thompson says there are no private-practice therapists in the county.
Challenging Times for Independent Operators
Luke Collins was the first person in his family born in a hospital. He served eight years as mayor of Clay County and last month was elected mayor of the town of Celina. He ran on a platform that advocated the reopening of Cumberland River Hospital.
Collins, like government officials across rural America, knows the economic consequences of a closed hospital. “The ripple effect is huge, and I don’t know how you would even measure it.”
Clay County advertises itself as the “Gateway to Dale Hollow Lake,” an attractive location for a retirement home. The absence of a hospital is a deterrent.
“I love this community and love this hospital,” Collins says. “It’s very, very important that we find a way to get this hospital back open.”
His ally in this effort is Johnny Presley. Presley is determined to reopen the hospital in Celina, and then those in Jamestown, Jellico and beyond.
Presley grew up in Crossville, an hour south of Celina. His passion for health care was sparked in his youth, riding in his dad’s tow truck responding to traffic accidents. He became a volunteer fireman, an EMT, then a physician assistant and health care administrator. He’s now on a mission to restore hospital care to the region. Some consider it a quixotic quest. Presley believes he can succeed.
In fact, he did temporarily reopen Cumberland River Hospital, in April 2020, just as the pandemic hit. There were issues. Presley cites the denial of COVID-19-related financial support from the state, delay in payment from insurance companies and the local EMS opting to transport patients to other hospitals. The hospital closed again in August.
These are challenging times for independent hospital operators. Alan Morgan, CEO of the National Rural Health Association, says federal requirements to “modernize health care and move toward electronic medical records created tremendous cost pressures” on small hospitals. “And those systems have to be updated yearly.”
Larger hospital systems are better positioned financially to access advanced technology. They also have greater purchasing power and the advantages of consolidated administration.
The Affordable Care Act put additional strains on rural hospitals – especially in states that haven’t yet expanded Medicaid – by limiting their ability to write off bad debt. Then came the pandemic, further diminishing at-risk margins.
“The pandemic made it much more difficult to be an independent rural hospital,” Morgan says, “and I think that’s going to be the case going forward.”
Reassessing Needs and Repurposing Appropriately
Twelve states have not yet adopted Medicaid expansion as allowed for under the Affordable Care Act. None of the eight states with the most rural hospital closures has implemented expansion. (Voters in two of those states, Missouri and Oklahoma, last year approved ballot measures to expand.) A 2018 study from the Colorado School of Public Health found that hospitals in non-expansion states are six times more likely to close than those in expansion states.
Six of those non-expansion states are in the Appalachian region, Tennessee among them.
A 2020 analysis of rural hospital financial and operational data by the Chartis Center for Rural Health found that more than half of Tennessee’s rural hospitals are performing at a level similar to that of rural hospitals that have closed since 2010.
“I don’t understand how we can continue to pass up those dollars,” the Rural Health Association of Tennessee’s Jacy Warrell says.
But, of course, Medicaid expansion isn’t a cure-all. Among the other primary issues that must be addressed is a workforce shortage. The average age of clinicians in rural communities is higher than nationally; attracting new providers is difficult. And Morgan says he’s hearing from rural hospital administrators that increasingly more nurses are leaving for higher-paying traveling-nurse positions.
The pandemic worsened the workforce shortage, with older practitioners, at greater risk of contracting the virus, choosing to retire.

In a report titled “The Ambulance Is Our Emergency Room,” the nonprofit Tennessee Health Care Campaign offers several recommendations for bolstering the state’s rural health care workforce. These include providing more state-funded loan-repayment opportunities for recent graduates as incentives to work in rural communities; incentivizing colleges and universities to reserve spots in their programs for rural residents; and expanding the reach of case managers, community health workers and in-home providers.
The THCC report was the outcome of listening sessions with community members throughout the state. Among its other recommendations is helping facilitate free-standing emergency rooms. In Tennessee, freestanding ERs must be hospital owned. The THCC suggests changing that policy, creating more opportunities for ERs to open in areas where hospitals have closed or aren’t financially viable.
And it urges the state to provide grant and investment opportunities to bolster primary, preventive, behavioral and oral care services in communities. Mountain People’s Health Councils, in Scott County, is a model of community-based services. It’s community owned, operating six clinics, including a new facility with pediatric care, behavioral health and dentistry.
The THCC report offers sound recommendations, but addressing the rural health crisis requires much more. It requires, first, says Richard Henighan, an east-Tennessee nurse practitioner and THCC board member, reassessing needs and repurposing appropriately.
“Some of these rural counties don’t need an old-fashioned rural hospital,” Henighan says.
The National Rural Health Association’s Morgan agrees: “I think in many communities, the need for inpatient beds is going to be minimal.” More services are now provided on an outpatient basis.

The focus, he says, should be on a 24/7 emergency room, primary care, general surgery and “a high reliance on telehealth,” then determining what else the community most needs – what services they would otherwise have to travel the farthest to receive.
Henighan says an important lesson he learned in conversations held while helping compile the THCC report was that reopening a hospital in a rural community “doesn’t necessarily mean the problem was fixed.” A broader issue, he says, is a failure to integrate services to meet the sum of a community’s health care needs.
A lasting solution requires addressing the social determinants of health, bringing together the hospital, clinics, local government agencies, business leaders, churches, civic clubs – the full resources of a community.
Morgan stresses that a successful rural hospital’s strategy must embrace preventive health and chronic-care management and “empowering the community to take control of their own health.”
‘The Answers Are There’
The federal CARES Act, passed by Congress to financially respond to the pandemic, provided an infusion of money to rural hospitals. Far more assistance is needed.
The THCC’s report asserts that “the state offers no assistance to rural community leaders to discourage hospital owners from closing the facility, finding a replacement administrative structure, or addressing the health needs after the loss.”
For Henighan, “the big disconnect” is that those being most harmed by the current state of health care continue to elect people who are ignoring them.
“Health care has become a political game with the leaders in our state,” says Michele Johnson, co-founder and executive director of the Tennessee Justice Center, referencing the refusal to expand Medicaid. “And the people who’ve paid the price for that are our rural communities.”
More fundamentally, Johnson believes “health care as a commodity violates who we are as a nation.” In her work, she sees firsthand “how that destroys lives and destroys families and communities.”
Robin Feierabend, a retired family physician in Bristol, Tennessee, is a member of a group called Physicians for a National Health Program. “Our whole health care system is currently so fragmented and so dysfunctional that I don’t think there are any simple solutions,” he says.

“But with a national health care plan, there’s the opportunity for much more coordination and oversight, and for matching of health care needs with populations, as opposed to our current competitive approach to providing services.”
In the meantime, Jacy Warrell remains optimistic. “I think what needs to happen is for policymakers and administrators to really listen to the needs of the community and become partners in solving these issues. I think the answers are there.”
Those who began queuing up before midnight in Jellico for the Remote Area Medical clinic’s offer of free health care would like some hard evidence of those answers. They’d like assurance of sustained hospital care. They’d like to know they haven’t been forgotten.
“Everything gets shut down,” says Charity, 23, of nearby LaFollette, who prefers not to give her last name. She’s the mother of three; she worries about her community’s future. “Nobody wants to come here.” Her concerns are well founded. Without such essential infrastructure as health care, many rural communities will cease to exist.
Andrea Haas is hoping Jellico Medical Center will soon be reopened, that people will no longer have to drive out of county for care, that her aunt can return to her job in the emergency room. “I’m hopin’ and prayin’,” she says.
This is the third story in Critical Condition, a three part series. Read more here.
This story was funded by the National Geographic Society. It also had financial support from the Economic Hardship Reporting Project.
Editor’s Note: This story was updated on July 21, 2021, to correct the city in which Robin Feierabend lives to Bristol, Tennessee.



