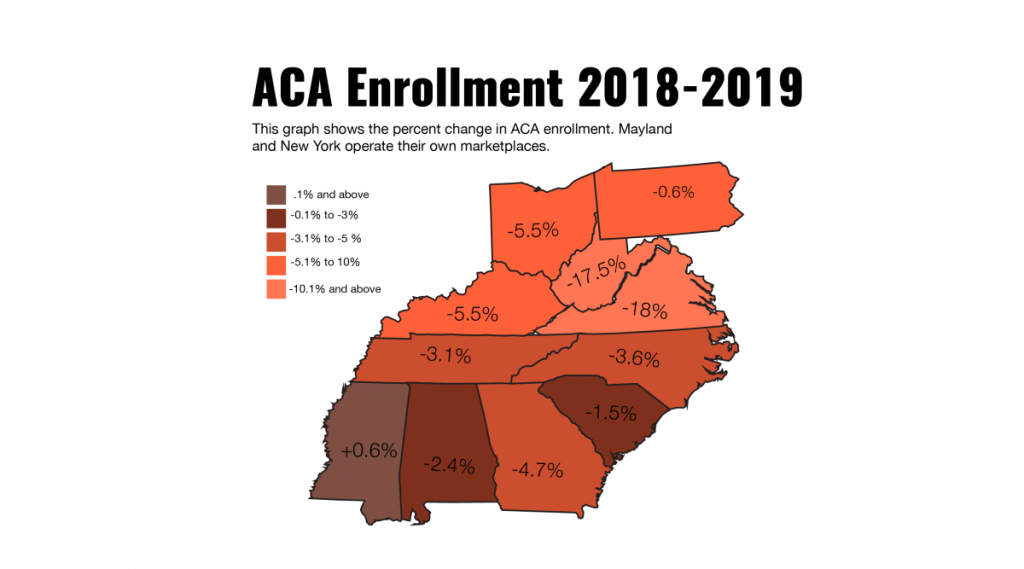
Fewer residents of Appalachia will have health insurance under the Affordable Care Act in 2019 than the year before. Enrollment numbers are down throughout the region, as they are nationwide, and some advocates say they aren’t surprised.
In 11 of the 13 Appalachian states that enroll residents through the federal HealthCare.gov website (Maryland and New York administer their own ACA marketplaces), only Mississippi saw a rise in enrollment numbers. West Virginia and Virginia saw the largest declines.
In West Virginia, some 22,600 residents signed up for or renewed health care policies under the ACA, as compared with about 27,400 for 2018, a 17.5 percent drop.
In 2017, 34,045 West Virginians were enrolled.
Of the 39 states that use HealthCare.gov for enrollment, the only that experienced a steeper decline was Virginia – but that was expected. As allowed for under the Affordable Care Act, Virginia expanded its Medicaid program in 2018, reducing the number of people in need of ACA coverage.
So if Virginia’s decline was anticipated due to changing health care policies in the state, what happened in West Virginia?
Kat Stoll said the primary factors are a reduction in spending for advertising and assistance, general confusion about the current and future state of the program and a stronger economy. Stoll is the policy director for West Virginians for Affordable Health Care, an advocacy group that works at the state and federal levels on health care issues that affect low-income consumers.
The advertising budget for the ACA under the Obama administration was more than $100 million a year nationally. The Trump administration slashed that budget by 90 percent.
Stoll believes this has a negative effect.
“People need that reminder,” she said, adding that “with media coverage of the ongoing repeal and replacement debate at the federal level,” the dissemination of information about the program helps clear up confusion.
“I was surprised by how many people thought the [ACA] was gone,” Stoll said.
She also pointed to the decline in spending for the state’s navigator assistance program, which provides in-person help in determining eligibility and financial assistance for health care coverage.
In 2017 in West Virginia, navigator programs administered by the West Virginia University Research Corporation and First Choice Health Systems received federal grants totaling $600,000. In 2018, those budgets were reduced to $100,000, an 83 percent cut. The Trump administration also cut budgets for navigator programs throughout the country.
Stoll cited a stronger economy as another potential source of the drop in enrollment numbers. The number of West Virginians eligible for Medicaid also declined. Both point to the assumption that more people are working, and may be receiving health care coverage through their employers.
“We were surprised to see the Medicaid enrollment drop,” she said. “We don’t think that was the result of any particular policies at the state level that presented barriers to eligibility for Medicaid. It might actually indicate some uptick in our economy, and that was reflected in some of the revenue estimates from the governor’s office.”
Stoll does not believe the Trump administration’s decision to remove the individual mandate, or the penalty for not having health insurance, was a big factor in the decline in numbers.
“I think people go to the marketplace to get the premium subsidy,” she said. “It’s more of a reward than a penalty system.”
Stoll said about 80 percent of West Virginians in the ACA marketplace receive a premium subsidy.
“I think the key to the marketplace’s success is getting the word out that there are premium subsidies available.”
Stoll cites one final curtailing factor in ACA enrollment: cost.
Cost is a factor for those at the higher-income levels of eligibility who don’t receive a subsidy, she said. And for those of lower-income, “even with generous subsidies, there are still out-of-pocket costs; there are still some premium costs. And when you’re dealing with a family right at that 150 percent of the poverty [level], having to spend perhaps a hundred bucks a month on insurance premiums and knowing you’re going to have copays – that’s a concern.”
“That’s a hard thing to squeeze into your family budget,” she added.
“Affordability has certainly been helped by the Affordable Care Act,” Stoll allowed, “but it’s not solved.”
Nationally, 8.4 million people enrolled or were automatically re-enrolled in an ACA health insurance plan during the 2019 open enrollment period; in 2018, that number was 8.7 million. But the drop wasn’t as precipitous as had been feared after a sluggish start to the six-week open-enrollment period. Enrollment picked up considerably in the final days.
Final enrollment data for 2019 to be released next month will include the results for those states that operate their own marketplace.



