Opioids and a rise in people experiencing homelessness have been blamed for a hepatitis A epidemic in West Virginia. But advocates for the homeless say the local census doesn’t support that.
West Virginia has been struggling with an outbreak of hepatitis A, according to local public health officials.
The most populous county in the state found itself the “major epicenter of a major hepatitis A outbreak,” said John Law, a public information officer at the Kanawha-Charleston Health Department (KCHD). Since March, West Virginia’s Department of Health and Human Resources (DHHR) has reported nearly 1,400 new cases of hepatitis A, an unprecedented increase. According to DHHR, the majority of the hepatitis A cases have been in Kanawha, Cabell and Putnam counties. Two cases have been reported in a northern West Virginia jail, and there have been at least two confirmed deaths.
Police and health officials say that the epidemic may be linked to a possible rise in people experiencing homelessness in West Virginia. But advocates for the homeless say the local census of people experiencing homelessness doesn’t support that theory. Others blame opioid usage for the state’s surging rates of hepatitis A.
Hepatitis A is a contagious disease often transmitted by food or water contaminated by fecal matter. People who are homeless or transient, those who don’t have access to proper sanitation, drug users, and the recently incarcerated may be at high risk, as well as anyone who has contact with higher-risk individuals. Symptoms of hepatitis A include whole body fatigue, fever, loss of appetite, diarrhea, nausea, and vomiting, as well as abdominal, joint, and muscle pain. Dark urine, itching, weight loss, and yellow skin and eyes (jaundice) are also common symptoms of infection.
The jump in West Virginia cases is alarming because, nationally, annual reports of hepatitis A cases have remained relatively stable, with a 95 percent decline since a vaccine became available in 1995, according to the Centers for Disease Control (CDC). Until this year, West Virginia reported an infection rate lower than or comparable to many other states. According to Janet Briscoe, the KCHD director of epidemiology, in an interview with local News Channel 3 WSAZ: “Before the outbreak, hepatitis A cases were rare in our region.” In 2010, previously the most recent year with the highest number of new cases, the state reported only 16 new cases.
Currently in West Virginia, “we are seeing it particularly in our homeless population. Maybe not the traditional on-the-street population, but the itinerate homeless—couch surfers,” Law of the DHHR said in an interview with Rewire.News. Those experiencing homelessness are at risk of hepatitis A due to the difficulty maintaining hygiene on the streets or without a permanent home.
Spotlight on Poverty and Opportunity, a nonpartisan forum on issues surrounding poverty in the nation, reports a total of more than 1,300 people experiencing homelessness in West Virginia, though it’s unclear how their count defines homelessness. An accurate, current count for both West Virginia and its capital proves hard to find because different agencies define homelessness differently.
As defined in a report from the Substance Abuse and Mental Health Services Administration, the point-in-time (PIT) count from the Department of Housing and Urban Development (HUD): “tallies the number of people in a community who are experiencing homelessness on a single night.” The PIT count taken in January for the entire state of West Virginia, according to the Western Virginia Continuum of Care, was higher than in years past, up by 9 percent, totaling 304 persons (including children) experiencing homelessness. But because of rural terrain and the difficulty reaching or finding many unknown people, this count may be low.
As reported in the Charleston Gazette-Mail, Charleston, West Virginia, Police Chief Steve Cooper stated last January there had been an influx of “several hundred” homeless people in the city and that homelessness in West Virginia is difficult to quantify.
This also makes linking the hepatitis A outbreak to homelessness difficult.
The outbreak in West Virginia “has been connected with the outbreaks in both California and Kentucky,” Law said. Though the original source of the infection remains unknown, researchers speculate that it first began in California, then spread. In addition to West Virginia, this year has seen newer outbreaks in Massachusetts, Missouri, Ohio, Arkansas, and Nashville, Tennessee.
According to Ellen Allen, executive director of Covenant House, a continuation of care site in Charleston that seeks to help the homeless through long-term support, PIT numbers have changed very little in the last five years—despite what is being claimed by the Charleston police department and mayoral office. “That’s not accurate at all. They know the homeless population has not tripled. This has been a point of contention with them,” she said in an interview with Rewire.News. She noted that local law enforcement have participated directly in the PIT count each year, which has stayed around 300 for Charleston.
Last month, a segment on News Channel 3 WSAZ ascribed an increase in the Charleston homeless population to people from out of state. According to Ronald Chandler, a man experiencing homelessness interviewed by WSAZ, many of these out-of-state individuals found their way to West Virginia after other states began to “crackdown” on the population.
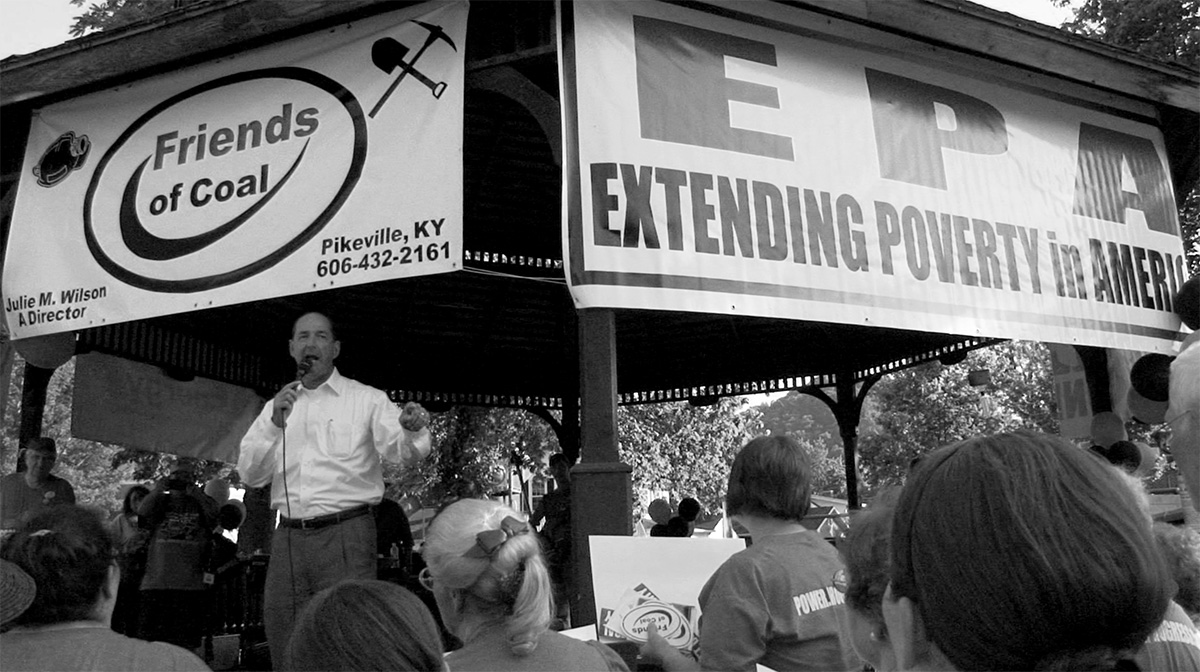
Allen disagrees, saying Covenant House sees many in the new homeless population coming from rural parts of West Virginia itself. “We’re not seeing them come from all over the country. We’re seeing them from areas like the devastated coal communities,” she said, noting Boone County as an example.
Nationally, numbers of people experiencing homelessness have been on the rise, with a 9 percent increase specifically in “unsheltered homelessness” in 2017 and 12 percent in “chronic homelessness” in 2017.
For Allen, community resources such as shelters serve as gatekeepers for the health of the high-risk population, offering access to resources like vaccines that some would not be able to easily obtain otherwise. “We try to respond collectively as a community, to get everyone immunized that we can,” Allen said. “We also know [the hepatitis A outbreak] is being driven by opioid addiction and we are arguably the epicenter of that as well.”
As of September 28, among the 1,395 hepatitis A cases in West Virginia, 76 percent report drug use, and 11 percent of the total number of people infected are considered homeless.
When it comes to individuals experiencing homelessness, “That particular population is sometimes difficult to access and make realize they need to be vaccinated and tested,” said Law. “We are reaching out to them in as many ways as we possibly can. For instance, we have provided vaccinations at shelters and soup kitchens.”
Because hepatitis A is a virus, treatment only addresses symptoms until the virus has run its course. The CDC, DHHR, and Law all urge those who qualify to prevent contracting the virus by getting vaccinated—though it’s a little more complicated than simply getting a shot, according to Law. “With hepatitis A, if you are vaccinated within two weeks of exposure, you will most certainly be protected against it. The dichotomy there is that you sometimes don’t manifest any symptoms until well after that two-week window.”
On August 25, the CDC distributed information to all state and local health departments about an investigation into hepatitis A infections specifically in people who are experiencing homelessness or who use illicit drugs.
At the end of August, West Virginia Public Broadcasting reported that at Gov. Jim Justice’s (R) request the CDC assigned six “subject matter experts” to “manage the outbreak,” assisting with technical tasks such as data management and case investigation strategies and procedures. The CDC’s Division of Viral Hepatitis has been monitoring and assisting many states since March 2017. The CDC did not respond to multiple requests from Rewire.News for comment.
“This outbreak is continuing; we have seen it across the country,” Law said. “The best thing is you can do, certainly, is to get vaccinated.”
According to a KCHD press release, in West Virginia “most adults have not been vaccinated for Hepatitis A.” Though beginning in 2006 the vaccine did become recommended vaccine, it is required only for children attending state preschool in West Virginia.
“The numbers we are seeing [of hepatitis A] have been lab-confirmed numbers. There is probably a larger number out there,” Law said. “These are the people who are sick enough to go to a health-care provider or hospital.”