After decades of addiction to heroin and prescription opioids, Wendy Crites finally made a clean break.
“For the first time in my life I just wanted to be off of it,” she said from her home in Ranson, West Virginia. “I hit rock bottom.”
Last year the ReSource profiled Crites, a single mother getting by on low-wage jobs during her first year of sobriety. Crites has had success with a combination of counseling and a medication called Suboxone.

“It’s been a huge part of my recovery,” she said. “I feel like the Suboxone has saved my life.”
Suboxone is a mixture of naloxone, the opioid-reversal medication, and a less potent opioid known as buprenorphine. It satisfies the brain’s craving for opioids without the body feeling the full effect of more powerful opioids.
Crites is among the thousands of people caught up in the Ohio Valley’s opioid crisis who find that treatment with medications such as Suboxone help them recover from addiction. But some face an obstacle on the road to recovery. Using the medication while driving can land them in trouble with the law. For Crites, that threatens the fragile gains she has made to better provide for her child and keep on the path to sobriety.
Maintaining Her Life
“When I met her she was renting a room that had no heat, during winter,” Rebecca Kiger recalled. Kiger, a photojournalist based in West Virginia, spent time with Crites documenting her struggle for sobriety, and the two have stayed in touch as Crites has improved her situation.
“She was working a minimum wage job at McDonald’s, she had no transportation but would ride a bike to work at all hours, including in the dark,” Kiger said.
“Since then I got my own place,” Crites said proudly in a recent interview with Kiger. “I got my license back, I got a car now.”
Kiger saw how important it was for Crites to have medication-assisted treatment.
“What it does for her, Wendy who has kind of lived with an addiction disorder since she was 15 years old, it allows her to not have her whole life focused around drug use,” Kiger said.
“I have not used heroin one time since I started taking Suboxone,” Crites said.
Kiger has seen how sobriety has changed Crites’ life and the lives of those around her.
“She can help her son get to school, help him study, hold down a full-time job, maintain relationships with her friends and family,” she said. “You know, maintain her life.”
Crites has been clean now for two years. But an incident in August could be her biggest challenge yet. Ironically, it has to do with the very medication that has helped keep her sober.
“I saw lights”
Crites said that a friend, another person in addiction recovery, asked her for a ride.
“Thirty seconds after I got him in the car I saw lights, got pulled over,” she said. The officer told her she had rolled through a stop sign, something she does not dispute. But what came after is what has her upset and worried about her future.
“When the officer saw who I was, he knew me,” she said.
The officer recognized Crites as someone he had once arrested in the days when she was in active addiction. He asked if there were drugs in the car.
“I said no, officer, I’ve been in the Suboxone program for two years and I don’t do drugs anymore.”
She allowed officers to search the vehicle. They found nothing.
“Then he asked, ‘So you said you’re in the Suboxone program?’” Crites recalled. “‘You will have to pass a field sobriety test.’”
Driving Problems
Suboxone has the potential to impair some drivers at certain doses. The safety information from Suboxone’s maker includes this warning: “Do not drive, operate heavy machinery, or perform any other dangerous activities until you know how Suboxone Film affects you.”
The company advises that buprenorphine, the main drug in Suboxone, “can cause drowsiness and slow reaction times during dose-adjustment periods.”
A study published in 2013 found slight impairment, especially among those not yet accustomed to the medication.

“At least some opioid maintenance therapy patients are observed having only slight impairments of relevance to driving,” the authors concluded.
Crites said she had been on the same prescribed dose for more than a year and was not impaired when she was pulled over. But when asked to stand on one foot, or walk heel-to-toe, she failed the sobriety test.
“I can’t do it. I am flat-footed and uncoordinated,” she said with a laugh. She also had recently recovered from a broken ankle in the past year, something Kiger documented during their time together.
Crites suspects there is another reason she was made to take a sobriety test.
A Catch-22
Crites said she thinks she was targeted because of her past and because of a stigma associated with Suboxone and other medication-assisted treatments for addiction.
“That’s how I messed up, I told him I take Suboxone,” Crites said of her encounter with the police.
Crites is not the only one who suspects law enforcement officers frequently take a dim view of Suboxone.
Public health experts call medication-assisted treatment, including use of Suboxone, the gold standard of addiction care. But outside of the clinical setting, Suboxone can also be abused and is sometimes diverted into the black market drug trade. That appears to color how police consider Suboxone users.
In her new book “Dopesick” author Beth Macy writes, “If you were drawing a Venn diagram comparing Suboxone attitudes among public health experts and criminal justice officials in Appalachian Bible-belt communities where the painkiller epidemic initially took root, the spheres would just barely touch.”
That disconnect between police and physicians is playing out on the region’s roads.
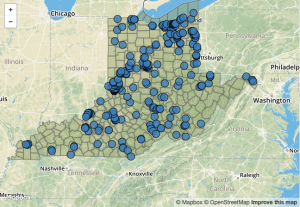
Dr. Jana Burson is a specialist in the treatment of opioid addiction working in North Carolina, where she also maintains a blog on issues that arise in treatment programs. In August Dr. Burson posted what she called “A Letter to Law Enforcement” about medication-assisted treatments and the number of her clients who were being pulled over on the highways.

“Dear Officer Zealous,” she began. “Please stop arresting my patients for whom I’ve prescribed methadone and buprenorphine …You mistakenly think all people taking these medications have no right to be driving, and you are wrong.”
Past Isn’t Dead
“I just wish people would get educated on Suboxone, that’s all,” Crites said with a sigh of exasperation, noting that her treatment is paid in part by the government.
“It’s like the state says ‘Okay, we need to help these people.’ But then the state penalizes you for it!” she said.
And in a small town where reputations matter, she feels she is still being punished for her past.
“It makes me angry that people can’t let you live down your past,” she said. “I’ve got so many people behind me who can say how much I changed my life, but there are people who can’t see past that.”
Crites is angry. She is also worried that she could lose her license, something that could jeopardize much of what she worked for in the past year. As Kiger learned in her time with Crites, she and her son live on a very thin margin.
“She faces paying a lot of fines, which can be crippling to someone who is in the economic category she’s in, which is basically working poor,” Kiger said.
Without transportation in a rural setting Crites would face difficulties getting her son to school and herself to work.
“I stand to lose everything, really,” Crites said. “My job, my home.”
And Kiger worries that Crites’ hard-won sobriety could also be at risk.
“It would be a real setback,” Kiger said. “After years of drug abuse, I would hate this to become a stress that has her turning to drugs to cope.”
Crites faces a preliminary court hearing in December. She said she will refuse a plea deal. But she does not yet have an attorney to offer her legal advice.
Crites applied for representation from the public defender’s office but found that with the slight raise she received from her new food service job the state considers her too wealthy for a court-appointed attorney.
This article was originally published by Ohio Valley Resource.



